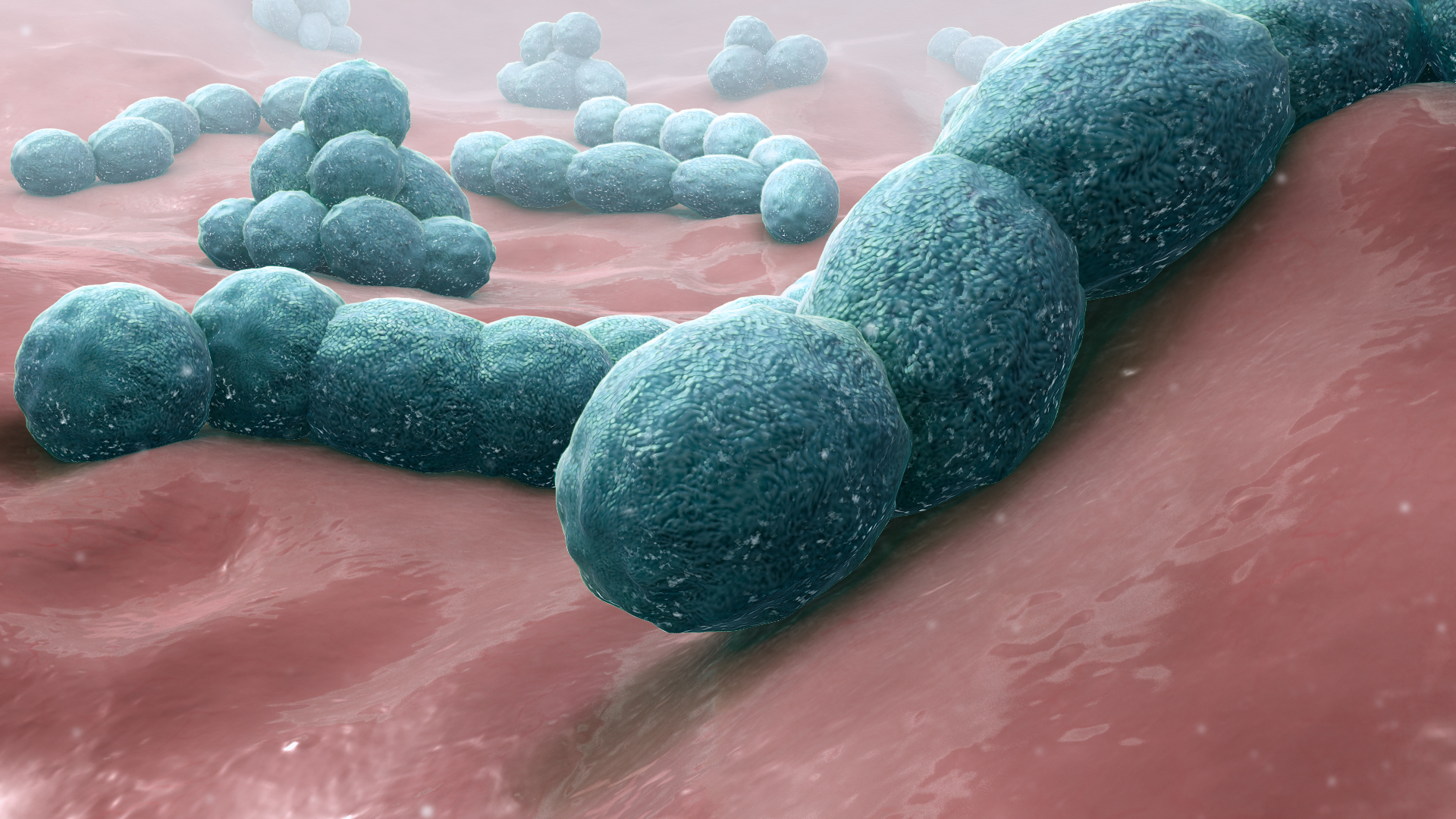
Streptococcus pneumoniae (or pneumococcus) is a type of bacteria that is a major cause of pneumonia – a disease where the lungs become inflamed and fill with fluid causing breathing difficulties. It’s more likely to be serious in the young, elderly or people with a weakened immune system.
In the UK alone pneumonia leads to around 40,000 people being hospitalised a year. Worldwide, pneumonia causes around 2.5 million deaths and is the single biggest cause of death in children living in low and middle income countries (LMIC). According to the World Health Organization, pneumonia was responsible for more than 920,000 childhood deaths in 2015.
There are vaccines available to protect people against pneumococcus – one that works better in children and one that is given to adults.
However, there are over 90 different types of these bacteria and the available vaccines only protect against certain strains. Furthermore, there are concerns that strains not covered by the vaccines might become more of a threat. So there is still a real need to develop better vaccines that protect more people from pneumococcus.
New research from Professor Daniela Ferreira’s team, based at the Liverpool School of Tropical Medicine, has uncovered new details about the immune response to pneumococcal infections, and could speed up the development of new and more effective vaccines. The research was published online in July 2019 in the Journal of Clinical Investigation.
Natural immunity could help develop a vaccine
While pneumococcus can cause very serious illness in some people, it mostly causes common and largely harmless infections. At any one time, as many as half of all young children and 1 in 10 adults are carrying the bacteria around in their noses and throats without any symptoms (called ‘carriage’). Carriage is important because it can lead to full-blown disease and is how the bacteria spreads between people.
- Dr Carla Solorzano-Gonzalez
For the majority of people who become colonised with pneumococcus, their immune system halts the spread of the infection and gets rid of the bugs. Immune cells have the ability to ‘remember’ bacteria, so the next time they are exposed to the germs they can deal with them straight away, protecting people from subsequent infections (‘immunity’).
Researchers want to uncover more details about the immune response to pneumococcus, to underpin the development of vaccines that could give children and vulnerable adults the same protective immunity without exposing them to potentially life-threatening bacteria.
To fully understand the battle between the bacteria and immune cells in people, researchers need to examine samples from the inside of peoples’ noses after they have been infected. And thanks to new research from Professor Ferreira’s team, they have shown how a human infection challenge study can provide this crucial detailed information.
The important first site of contact
The team have carried out human infections studies before, where they ask healthy adults to volunteer to be infected with pneumococcus so they can study the immune response. One of the lead researchers in the team, Dr Carla Solorzano-Gonzalez, explains what was new and exciting about this study.
“We are particularly interested in what happens at the site of first contact with the bacteria – the inside of the nose,” she says.
In previous studies we have scooped a little bit of the nose lining out, but we don’t get many cells by doing it that way. This is the first study we have worked with a specialist surgeon, Dr. Sam Leong, to help us safely take small biopsies instead. Taking samples this way gives us much more information.”
The study involved 20 adult volunteers – the medical checks beforehand confirmed they were all healthy and at very low risk of becoming seriously ill from pneumococcus bacteria.
“We also tested them to make sure they weren’t already carrying a type of pneumococcus in their noses before the study” says Dr Solorzano-Gonzalez. “Then we gave the volunteers a dose of a pneumococcus strain that can be easily treated with antibiotics, using nose drops, which mimics how the bacteria would normally get into our bodies.”
The researchers tested nose washings from the volunteers 2 and 7 days after they were exposed, to find out if the bacteria had established an infection.
“From the 20 volunteers we exposed, or “challenged”, 8 became infected,” says Dr Solorzano-Gonzalez. “The remaining 12 volunteers already had protective immunity, likely because of their previous natural exposures to this bacteria, as we are all in contact with it from time to time.
A week after exposure, we gave everyone antibiotics to kill the bacteria, whether we had detected them in the nose washings or not. Then, once the antibiotics had worked, we took a small biopsy under local anaesthetic from the noses of our volunteers.”
A rich tapestry of detail
Taking a biopsy allowed the researchers to reveal a huge amount of detail about the immune cells in the noses of people who became infected compared to those who didn’t.

- Dr Carla Solorzano-Gonzalez
“We used a technique called CyTOF,” says Dr Solorzano-Gonzalez. “It uses trace amounts of heavy metals and allows us to get huge amounts of details about each individual cell. We did this in collaboration with Leiden University Medical Center.”
The team found two details that could be important for understanding which specific branches of the immune system are important in giving people immunity to pneumococcus infections.
“Firstly, we noticed that people that were protected had higher types of a particular immune cells, called a ‘CD8 MAIT cell’ in their noses.
We think these cells are important in the early immune response to the bacteria – they signal to other immune cells that something is wrong and kick-start the defence systems. But they also might be important for the process of “remembering” the bacteria and giving people long-lasting protection.”
This was a surprising finding for the team, because it had previously been thought from research involving animals that other types of white blood cells were more important.
“We also found that people who became infected had lower levels of a type of cell called a B cell in their noses post infection. The B cells had activated and entered the blood stream to produce antibodies to fight the infection.
In comparison, previous studies conducted in our team have shown that volunteers who are protected after exposure, have higher numbers of memory B cells (immune cells that specifically remember pneumococcus) to start with. So we think B cells might also be important for giving people long-lasting immunity.”
A step towards better vaccines
This research is a first step towards understand natural immunity to pneumococcal infection and what is important in protecting people.
“Once we understand natural immunity, and which parts correlate with protection against disease, we can apply this knowledge to designing better vaccines that generate the same protection,” says Dr Solorzano-Gonzalez.
It might also shed light on other bacterial infections and the immune response to them too, potentially underpinning vaccines to other diseases as well.
“We can’t thank the volunteers enough – thanks to them being willing to take part in studies like this, we might be on the way to better vaccines, which will save many lives around the world.”